TUBERCULOSIS:
- Tuberculosis: Learn the Signs and Symptoms of TB Disease:
TB is a disease caused by bacteria that are spread from person to person through the air. TB disease usually occurs in the lungs, but it can also occur in other parts of the body, such as the brain, the kidneys, or the spine.
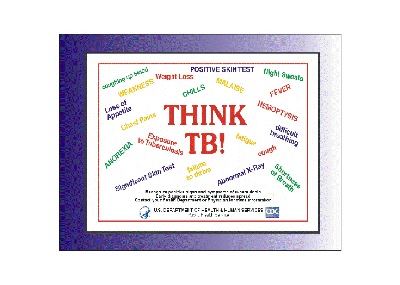
. Symptoms of TB disease depend on where in the body the TB bacteria are growing. TB disease in the lungs may cause symptoms such as A bad cough that lasts 3 weeks or longer
· Pain in the chest
· Coughing up blood or sputum (phlegm from deep inside the lungs)
Other symptoms of active TB disease are:
· Weakness or fatigue
· Weight loss
· No appetite
· Chills
· Fever
· Sweating at night
Other symptoms of active TB disease are:
· Weakness or fatigue
· Weight loss
· No appetite
· Chills
· Fever
· Sweating at night
You should get tested for TB if:
· You have spent time with a person known to have TB disease or suspected to have TB disease; or
· You have HIV infection or another condition that puts you at high risk for developing TB disease; or
· You think you might have TB disease; or
· You are from a country where TB disease is common (most countries in Latin America and the Caribbean, Africa, Asia, Eastern Europe, and Russia); or
· You live in a place where TB disease is more common such as a homeless shelter, migrant farm camp, prison or jail, and some nursing homes); or
· You inject illegal drugs
· If you think you may have been exposed to a person with TB disease, contact your health care provider or your state or local TB control office.
Basic TB Facts
How TB SpreadsLatent TB Infection & TB DiseaseThe Difference Between Latent TB Infection & TB DiseaseRelated Links
"TB" is short for tuberculosis. TB disease is caused by a bacterium called Mycobacterium tuberculosis. The bacteria usually attack the lungs, but TB bacteria can attack any part of the body such as the kidney, spine, and brain. If not treated properly, TB disease can be fatal.
- How TB Spreads:
TB is spread through the air from one person to another. The TB bacteria are put into the air when a person with active TB disease of the lungs or throat coughs, sneezes, speaks, or sings. People nearby may breathe in these bacteria and become infected.
TB is NOT spread by
· shaking someone’s hand
· sharing food or drink
· touching bed linens or toilet seats
· sharing toothbrushes
· kissing
- Latent TB Infection and TB Disease:
Not everyone infected with TB bacteria becomes sick. As a result, two TB-related conditions exist: latent TB infection and active TB disease.
- Latent TB Infection:
TB bacteria can live in your body without making you sick. This is called latent TB infection (LTBI). In most people who breathe in TB bacteria and become infected, the body is able to fight the bacteria to stop them from growing. People with latent TB infection do not feel sick and do not have any symptoms. The only sign of TB infection is a positive reaction to the tuberculin skin test or special TB blood test. People with latent TB infection are not infectious and cannot spread TB bacteria to others. However, if TB bacteria become active in the body and multiply, the person will get sick with TB disease.
- TB Disease:
TB bacteria become active if the immune system can't stop them from growing. When TB bacteria are active (multiplying in your body), this is called TB disease. TB disease will make you sick. People with TB disease may spread the bacteria to people they spend time with every day. Many people who have latent TB infection never develop TB disease. Some people develop TB disease soon after becoming infected (within weeks) before their immune system can fight the TB bacteria. Other people may get sick years later, when their immune system becomes weak for another reason.
For persons whose immune systems are weak, especially those with HIV infection, the risk of developing TB disease is much higher than for persons with normal immune systems.
- How TB Spreads:
TB is spread through the air from one person to another. The TB bacteria are put into the air when a person with active TB disease of the lungs or throat coughs, sneezes, speaks, or sings. People nearby may breathe in these bacteria and become infected.
- TB is NOT spread by:
shaking someone’s hand, sharing food or drink, touching bed linens or toilet seats, sharing toothbrushes, AND kissing.
- Latent TB Infection and TB Disease:
Not everyone infected with TB bacteria becomes sick. As a result, two TB-related conditions exist: latent TB infection and active TB disease.
- Latent TB Infection:
TB bacteria can live in your body without making you sick. This is called latent TB infection (LTBI). In most people who breathe in TB bacteria and become infected, the body is able to fight the bacteria to stop them from growing. People with latent TB infection do not feel sick and do not have any symptoms. The only sign of TB infection is a positive reaction to the tuberculin skin test or special TB blood test. People with latent TB infection are not infectious and cannot spread TB bacteria to others. However, if TB bacteria become active in the body and multiply, the person will get sick with TB disease.
- TB Disease:
TB bacteria become active if the immune system can't stop them from growing. When TB bacteria are active (multiplying in your body), this is called TB disease. TB disease will make you sick. People with TB disease may spread the bacteria to people they spend time with every day. Many people who have latent TB infection never develop TB disease. Some people develop TB disease soon after becoming infected (within weeks) before their immune system can fight the TB bacteria. Other people may get sick years later, when their immune system becomes weak for another reason.
For persons whose immune systems are weak, especially those with HIV infection, the risk of developing TB disease is much higher than for persons with normal immune systems.
- The Difference between Latent TB Infection and TB Disease:
A Person with Latent TB Infection
• Has no symptoms • Does not feel sick • Cannot spread TB bacteria to others • Usually has a skin test or blood test result indicating TB infection • Has a normal chest x-ray and a negative sputum smear • Needs treatment for latent TB infection to prevent active TB disease
- A Person with TB Disease:
• Has symptoms that may include:
- a bad cough that lasts 3 weeks or longer
- pain in the chest
- coughing up blood or sputum
- weakness or fatigue
- weight loss
- no appetite
- chills
- fever
- sweating at night
• Usually feels sick,
• May spread TB bacteria to others • Usually has a skin test or blood test result indicating TB infection • May have an abnormal chest x-ray, or positive sputum smear or culture • Needs treatment to treat active TB disease
- Treatment for Latent TB Infection (LTBI):
People with latent TB infection have TB germs in their bodies, but they are not sick because the germs are not active. These people do not have symptoms of TB disease, and they cannot spread the germs to others. However, they may develop TB disease in the future. They are often prescribed treatment to prevent them from developing TB disease. Because there are less bacteria in a person with latent TB infection, treatment is much easier. Usually, only one drug is needed to treat latent TB infection. The medicine usually taken for the treatment of latent TB infection is called isoniazid (INH). INH for 9 months is the preferred regimen. INH kills the TB bacteria that are in the body. Children and people with HIV infection may need to take INH for a longer time.
- Treatment for TB Disease:
A person with active TB disease has a large amount of TB bacteria in the body. TB disease can be treated by taking several drugs for 6 to 12 months. It is very important that people who have TB disease finish the medicine, and take the drugs exactly as prescribed. If they stop taking the drugs too soon, they can become sick again; if they do not take the drugs correctly, the germs that are still alive may become resistant to those drugs. TB that is resistant to drugs is harder and more expensive to treat.
- Infection Control and Prevention, Infection Control in Health Care Settings:
All health care settings need an infection-control program designed to ensure prompt detection, airborne precautions, and treatment of persons who have suspected or confirmed TB disease. In order to be effective, the primary emphasis of the TB infection-control program should be on achieving these three goals.
In all health-care settings, particularly those in which persons are at high risk for exposure, policies and procedures for TB control should be developed, reviewed periodically, and evaluated for effectiveness to determine the actions necessary to minimize the risk for transmission of TB.Infection Control in Health-Care Settings (Fact sheet)Respiratory Protection in Health-Care Settings (Fact sheet)
- What to Do If You Have Been Exposed to TB:
If you think you have been exposed to someone with TB disease, you should contact your doctor or local health department about getting a TB skin test or a special TB blood test. Be sure to tell the doctor or nurse when you spent time with the person who has TB.More: What to Do If You Have Been Exposed to TB
- Preventing Latent TB Infection from Progressing to TB Disease:
Many people who have latent TB infection never develop active TB disease. But some people who have latent TB infection are more likely to develop active TB disease than others. Those at high risk for developing active TB disease include:
People with HIV infection, People who became infected with TB bacteria in the last 2 years, Babies and young children, People who inject illegal drugs, People who are sick with other diseases that weaken the immune system, Elderly people, People who were not treated correctly for TB in the past.
If you have latent TB infection and you are in one of these high-risk groups, you need to take medicine to keep from developing active TB disease. This is called treatment for latent TB infection. There are several treatment options. You and your health care provider must decide which treatment is best for you. If you take your medicine as instructed by your doctor or nurse, it can keep you from developing active TB disease. Because there are less bacteria, treatment for latent TB infection is much easier than treatment for TB disease. A person with active TB disease has a large amount of TB bacteria in the body. Several drugs are needed to treat active TB disease.
- Preventing Exposure to TB Disease While Traveling Abroad:
Travelers should avoid close contact or prolonged time with known TB patients in crowded, enclosed environments (for example, clinics, hospitals, prisons, or homeless shelters).
Travelers who will be working in clinics, hospitals, or other health care settings where TB patients are likely to be encountered should consult infection control or occupational health experts. They should ask about administrative and environmental procedures for preventing exposure to TB. Once those procedures are implemented, additional measures could include using personal respiratory protective devices.
