Healthcare Wide Hazards.
All provided information supports the fact that Federal, State Laws must be followed without exception of fact. All facility policy and procedures must be followed. In the event of exception to fact, contact your direct NurseLine Healthcare Supervisor and the facility supervisor for direction.
We are currently creating content for this section. In order to be able to keep up with our high standards of service, we need a little more time. Please stop by again. Thank you for your interest!
Employee exposure to bloodborne pathogens from blood and Other Potentially Infectious Materials (OPIM) because employees are not using Universal Precautions. Bloodborne pathogens are pathogenic microorganisms that are present in human blood and can cause disease in humans.
Some infections that can be transmitted through contact with blood and body fluids include:
HIV, Hepatitis A, B, C, Staph and Strep infections, Gastroenteritis-salmonella, and shigella, Pneumonia, Syphilis, TB, Malaria, Measles, Chicken Pox, Herpes, Urinary tract infections, and Blood infections. The greatest risks are from HIV and Hepatitis B and C.
<B>Healthcare-associated Infections (HAIs)</B>:
Healthcare-associated infections (HAIs) are infections caused by a wide variety of common and unusual bacteria, fungi, and viruses during the course of receiving medical care.
Medical advances have brought lifesaving care to patients in need, yet many of those advances come with a risk of HAI. These infections related to medical care can be devastating and even deadly. As our ability to prevent HAIs grows, these infections are increasingly unacceptable.
Recent successes in HAI elimination have been very encouraging. Examples include sustained reduction in central line-associated bloodstream infections (CLABSIs) by 70%, simply by ensuring adherence to available guidelines. Reductions have been demonstrated for other HAIs as well, but, much more remains to be done.
Wherever patient care is provided, adherence to infection prevention guidelines is needed to ensure that all care is safe care. This includes traditional hospital settings as well as outpatient surgery centers, long-term care facilities, rehabilitation centers, and community clinics. The information on this website is intended to inform patients and healthcare personnel and help move healthcare systems toward elimination of HAIs.
Universal PrecautionsDefinition:
Universal precautions are safety procedures established by the Centers for Disease Control and Prevention (CDC) and the American Dental Association (ADA).Purpose
These precautions are used in medical and dental offices to prevent the transmission of infectious diseases to patients and health care workers.Description
Universal precautions are standards of infection control practices designed to reduce the risk of transmission of bloodborne infections.Personal protective equipment
Protective equipment includes gloves, gowns, masks, and eyewear worn by health care workers to reduce the risk of exposure to potentially infectious materials.
Examination gloves are used for procedures involving contact with mucous membranes. They reduce the incidence of contamination to the hands, but they cannot prevent penetrating injuries from needles or other sharp instruments. Gloves are changed after each patient and discarded, and must never be washed or disinfected for reuse. Washing with surfactants may cause wicking (the enhanced penetration of liquids through undetected holes in the glove). Disinfecting agents may cause deterioration of the gloves. Petroleum jelly may also break down latex. Utility gloves may be used when handling contaminated instruments and cleaning of the treatment area or sterilization room.
Fluid-resistant gowns, laboratory coats, or uniforms should be worn when clothing is likely to be soiled with blood or other bodily fluids. Reusable protective clothing should be washed separately from other clothes, using a normal laundry cycle. Protective clothing should be changed daily or as soon as visibly soiled. They should be removed before personnel leave areas of the dental office used for laboratory or patient-care activities.
Masks and protective eyewear, or chin-length, plastic face shields should be worn when splashing or spattering of blood or other body fluids is likely. A mask should be changed between patients or during patient treatment if it becomes wet or moist. A face shield or protective eyewear should be washed with appropriate cleaning agents when visibly soiled.Careful handling and disposal of sharps
Sharp disposable items, such as needles, saliva ejectors, rubber prophy cups and scalpels that cannot be sterilized and are contaminated with blood or other body fluids need to be discarded in puncture resistant containers. Special delivery companies pick up the containers once they are full and replace them with empty containers.Careful handling and cleaning of contaminated equipment
Dental instruments must be cleaned and sterilized after each use. Recommended sterilization methods include autoclaving or using a dry heat oven or "chemiclave," a unit that cleans with the use of chemicals. Sterilization equipment is commonly found in a special area of the building away from the treatment areas.
Cleaning and disinfecting of all surfaces such as lights, drawer handles, and countertops is accomplished by a chemical solution formulated to kill infectious bacteria, spores, and viruses after each patient is seen. Medical facilities follow specific heat sterilization procedures, which are outlined by the CDC. Plastic barriers cover items that are not easily disinfected by chemical spray, such as light handles, chair control buttons, and instrument trays. Many offices and hospitals have seamless floors with linoleum or a laminate surface so that spills can be contained and cleaned quickly.
Non-critical items that cannot be heat sterilized are sterilized by chemical immersion formulated to kill infectious bacteria and viruses.
Universal precautions are intended to supplement rather than replace recommendations for routine infection control, such as hand washing.Preparation
Proper planning and management of supplies needed for universal precautions are essential in reducing the occupational risk of infectious diseases. Such measures should include, but are not limited to:
- risk assessment
- setting of standards and protocols
- risk reduction
- post-exposure measures
- first aid
Complications:
Complications include the possible increase of medical and dental fees to the patient to offset costs associated with the equipment, disinfectants, and sterilization procedures needed for universal precautions.Results
Universal precautions are designed to result in the reduction of the transmission of infectious diseases to patients and health care workers.Health care team roles
Universal precautions require all medical and dental staff personnel involved in patient care to use appropriate personal protective equipment. Guidelines for health care settings for discarding of waste material are under a separate code by individual state agencies and governmental departments.
The environment in which health care is provided is greatly affected by universal precautions, both for the patient and care providers. Measures that promote a safe work environment include:
- education of employees about occupational risks and methods of prevention of HIV and other infectious diseases
- provision of protective equipment
- provision of appropriate disinfectants to clean up spills of blood or other body fluids
- easy accessibility of puncture-resistant sharps containers
- maintaining appropriate staffing levels
- measures that reduce and prevent stress, isolation, and burnout
- controlling shift lengths
- providing post-exposure counseling, treatment, and follow-up
The U.S. Department of Labor Occupational Safety and Health Administration (OSHA) requires employers in the medical and dental fields to make hepatitis B virus (HBV) vaccines available without cost to employees who may be exposed to blood or other infectious materials. In
addition, the CDC recommends that all workers be vaccinated against HBV, as well as influenza, measles, mumps, rubella, and tetanus, both for the protection of personnel and patients.
KEY TERMS:
Autoclave—A sterilization unit that uses steam under pressure.
Chemiclave—A sterilization unit that uses chemicals under pressure.
Dry heat oven—A sterilization unit that uses dry heat.
Sharps—Needles and cutting instruments such as curets and scalpel blades.
Possible Solutions:
Use Universal Precautions. Universal precautions is an approach to infection control to treat all human blood and certain human body fluids as if they were known to be infectious for HIV, HBV and other bloodborne pathogens, (Bloodborne Pathogens Standard 29 CFR 1910.1030(b) definitions). Bloodborne Pathogen Standard 29 CFR 1910.1030(d)(1) requires:
Employees to observe Universal Precautions to prevent contact with blood or other potentially infectious materials (OPIM).
Under circumstances in which differentiation between body fluid types is difficult or impossible, all body fluids shall be considered potentially infectious materials.
Treat all blood and other potentially infectious materials with appropriate precautions such as:
Use gloves, masks, and gowns if blood or OPIM exposure is anticipated.
Use engineering and work practice controls to limit exposure. OPIM is defined in 29 CFR 1910.1030(b) as: The following human body fluids: semen, vaginal secretions, cerebrospinal fluid, synovial fluid, pleural fluid, pericardial fluid, peritoneal fluid, amniotic fluid, saliva in dental procedures, any body fluid that is visibly contaminated with blood, and all body fluids in situations where it is difficult or impossible to differentiate between body fluids;
Any unfixed tissue or organ (other than intact skin) from a human (living or dead); and
HIV-containing cell or tissue cultures, organ cultures, and HIV- or HBV-containing culture medium or other solutions; and blood, organs, or other tissues from experimental animals infected with HIV or HBV. The Bloodborne Pathogens Standard allows for hospitals to use acceptable alternatives [OSHA Directive CPL 02-02-069] to universal precautions: Alternative concepts in infection control are called Body Substance Isolation (BSI) and Standard Precautions. These methods define all body fluids and substances as infectious. These methods incorporate not only the fluids and materials covered by the Bloodborne Pathogens Standard but expands coverage to include all body fluids and substances.
These concepts are acceptable alternatives to universal precautions, provided that facilities utilizing them adhere to all other provisions of the standard.
For compliance with OSHA Standards, the use of either Universal Precautions or Standard Precautions are acceptable. The CDC recommends Standard Precautions for the care of all patients, regardless of their diagnosis or presumed infection status. Standard Precautions apply to 1) blood; 2) all body fluids, secretions, and excretions, except sweat, regardless of whether or not they contain visible blood; 3) non-intact skin; and 4) mucous membranes. Standard precautions are designed to reduce the risk of transmission of microorganisms from both recognized and unrecognized sources of infection in hospitals.
Standard precautions includes the use of: hand washing, appropriate personal protective equipment such as gloves, gowns, masks, whenever touching or exposure to patients' body fluids is anticipated. Transmission-Based Precautions (i.e., Airborne Precautions, Droplet Precautions, and Contact Precautions), are recommended to provide additional precautions beyond Standard Precautions to interrupt transmission of pathogens in hospitals.
Transmission-based precautions can be used for patients with known or suspected to be infected or colonized with epidemiologically important pathogens that can be transmitted by airborne or droplet transmission or by contact with dry skin or contaminated surfaces. These precautions should be used in addition to standard precautions.
Airborne Precautions used for infections spread in small particles in the air such as chicken pox.
Droplet Precautions used for infections spread in large droplets by coughing, talking, or sneezing such as influenza.
Contact Precautions used for infections spread by skin to skin contact or contact with other surfaces such as herpes simplex virus. Airborne Precautions, Droplet Precautions, and Contact Precautions. May be combined for diseases that have multiple routes of transmission. When used either singularly or in combination, they are to be used in addition to Standard Precautions. For additional information, see HealthCare Wide Hazards - Needlesticks.
Additional Information: http://www.osha.gov/pls/oshaweb/owaredirect.html?p_url=http://www.cdc.gov/ncidod/dhqp/gl_isolation.html. Centers for Disease Control and Prevention (CDC), Division of Healthcare Quality Promotion, (2007). Guidelines for Infection Control in Healthcare Personnel. Centers for Disease Control and Prevention (CDC), Division of Healthcare Quality Promotion, (1998). Bloodborne Infectious Diseases HIV/AIDS, Hepatitis B Virus, and Hepatitis C Virus. U.S. Department of Health and Human Services (DHHS), National Institute for Occupational Safety and Health (NIOSH).
Universal Precautions-continued:
An approach to infection control which treats all human blood and other potentially infectious materials as if they were known to be infectious for HIV, HBV or other bloodborne pathogens. [29 CFR 1910.1030(b)]
Potential Hazard
Exposure to bloodborne pathogens due to lack of universal precautions. Possible Solutions
Employer should implement universal precautions. [29 CFR 1910.1030(d)(1)]
Treat all blood and other potentially infectious materials with appropriate precautions.
Use gloves, masks, and gowns if blood or OPIM exposure is anticipated. Use engineering and work practice controls to limit exposure.
There are other concepts in infection control that are acceptable alternatives to universal precautions, such as Body Substance Isolation (BSI) and Standard Precautions [OSHA Directive CPL 02-02-069 (CPL 2-2.69), (2001, November 27)]. These methods define all body fluids and substances as infectious and incorporate not only the fluid and materials covered by the Bloodborne Pathogens Standard, but expand coverage to include all body fluids and substances.
For additional information, see Healthcare Wide Hazards - <B>Universal Precautions</B>.
ELECTRICAL UNIVERSAL PRECAUTIONS:
Preventing Electrocutions by Undetected Feedback Electrical Energy Present in Power Lines The potential for electrocution because of feedback electrical energy should not be underestimated. NIOSH investigations indicate that workers may not be aware of the extreme danger of electrocution and electrical injuries associated with feedback energy. These cases demonstrate that the problem of feedback electrical energy in electrical transmission and distribution systems is always present and that diligent efforts should be applied to safeguard against it. "Fuzzing" a line is a standard practice to test for the presence of high voltage in power lines. "Fuzzing" is accomplished by bringing a metallic object, such as a pair of lineman's pliers, close to a power line while watching for an arc and listening for a buzzing sound. This method does not reliably detect low voltages and should not be used as the only test for electrical energy in power lines. Once fuzzing has determined that high voltage is not present, low voltage testing equipment, such as a glowing neon light or a light-emitting diode, should be used to determine whether low voltage is present. RECOMMENDATIONS
The following NIOSH recommendations should substantially reduce the number of electrocutions caused by undetected feedback electrical energy in power lines. Particular emphasis should be placed on the first two recommendations. Universal Precautions Extreme caution must be exercised by persons working on or in the vicinity of unverified deenergized power lines. All persons performing this work should treat all power lines as "hot" unless they positively know these lines are properly deenergized and grounded. Persons should also be instructed that "fuzzing," although an accepted practice to check for high voltage in power lines, is not a reliable test method. As reported in Case No. 1, lower voltage levels can be deadly, and may not be detected by the practice of "fuzzing." "Fuzzing" must be done only after power lines have been deenergized and properly grounded. Because of the possibility of a feedback circuit, the person performing the work should personally ground all lines on both sides of the work area unless he/she is wearing the proper protective equipment. Training Programs Training programs for linemen should emphasize proper procedures for working with electrical transmission and distribution systems and their associated dangers. Training programs for linemen should include basic electrical theory that addresses electrical distribution systems and the identification, evaluation, and control of the dangers associated with these systems. Because the danger of feedback energy is always present, an improved method of deenergizing these systems should be stressed. Protective Equipment and Work Practices Power lines should not be repaired or otherwise accessed without adequate Personal safety equipment unless the worker personally verifies that the line is deenergized and properly grounded. Workers must be specifically instructed to wear proper protective equipment, such as gloves and sleeves, required for the task to be performed. Linemen must be instructed to treat all power lines as energized unless they personally deenergize them by establishing a visible open point between the load and supply sides of the line to be repaired, by opening a fused disconnect, by opening a fused switch, or by removing a tap jumper if the load permits. Workers must verify that the power lines have been deenergized. Workers must provide proper grounding for the lines. Unless a power line is effectively grounded on both sides of a work area, it must be considered energized even though the line has been deenergized. Lines must be grounded to the system neutral. Grounds must be attached to the system neutral first and removed from the system neutral last. If work is being performed on a multiphase system, grounds must be placed on all lines. Lines should be grounded in sight of the working area and work should be performed between the grounds whenever possible. If work is to be performed out of sight of the point where the line has been deenergized, an additional ground should be placed on all lines on the source side of the work area. Detection of Low Voltage Persons working on or in the vicinity of power lines should be provided with appropriate safety and protective equipment and trained in procedures that address all magnitudes of voltages to which they may be exposed. Procedures should be established to perform a dual voltage check on the grounded load and supply sides of the open circuit. Once the "fuzzing" method has determined that high voltage is not present, low voltage testing equipment, such as a glowing neon light or a light-emitting diode, should be used to determine if lower voltage is present.
RECOMMENDATIONS:
The following NIOSH recommendations should substantially reduce the number of electrocutions caused by undetected feedback electrical energy in power lines. Particular emphasis should be placed on the first two recommendations.
Universal Precautions:
Extreme caution must be exercised by persons working on or in the vicinity of unverified deenergized power lines. All persons performing this work should treat all power lines as "hot" unless they positively know these lines are properly deenergized and grounded. Persons should also be instructed that "fuzzing," although an accepted practice to check for high voltage in power lines, is not a reliable test method. As reported in Case No. 1, lower voltage levels can be deadly, and may not be detected by the practice of "fuzzing." "Fuzzing" must be done only after power lines have been deenergized and properly grounded. Because of the possibility of a feedback circuit, the person performing the work should personally ground all lines on both sides of the work area unless he/she is wearing the proper protective equipment.
Training Programs:
Training programs for linemen should emphasize proper procedures for working with electrical transmission and distribution systems and their associated dangers. Training programs for linemen should include basic electrical theory that addresses electrical distribution systems and the identification, evaluation, and control of the dangers associated with these systems. Because the danger of feedback energy is always present, an improved method of deenergizing these systems should be stressed.
Healthcare Wide Hazards , Electrical CONTINUED:
Potential Hazard:
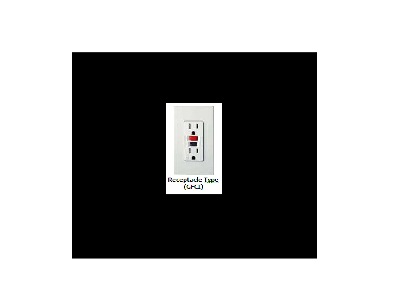
Employee exposure to electrical hazards including electric shock, electrocutions fires, and explosions. Damaged electrical cords can lead to possible shocks or electrocutions. A flexible electrical cord may be damaged by door or window edges, by staples and fastenings, by equipment rolling over it, or simply by aging.Possible electrocution or electric shock or contact with electrical hazards from:
· Faulty electrical equipment/machinery or wiring.
· Damaged receptacles and connectors.
· Unsafe work practices.
Possible Solutions
Comply with OSHA Standard 29 CFR 1910 Subpart S - Electrical. The standard is comprehensive and includes the following sections:
Electrical equipment shall be free from recognized hazards [29 CFR 1910.303(b)(1)].Listed or labeled equipment shall be used or installed in accordance with any instructions included in the listing or labeling [29 CFR 1910.303(b)(2)].Sufficient access and working space shall be provided and maintained around all electric equipment to permit ready and safe operation and maintenance of such equipment [29 CFR 1910.303(g)(1)].Ensure that all electrical service near sources of water is properly grounded [29 CFR 1910.304(g)(6)(vi)].Tag out and remove from service all damaged receptacles and portable electrical equipment [29 CFR 1910.334(a)(2)(ii)].Repair all damaged receptacles and portable electrical equipment before placing them back into service [29 CFR 1910.334(a)(2)(ii)].Ensure that employees are trained not to plug or unplug energized equipment when their hands are wet [29 CFR 1910.334(a)(5)(i)].Use safeguards for personnel protection and electrical protective equipment [29 CFR 1910.335(b)].Select and use appropriate work practices [1910.333].Follow requirements for Hazardous Classified Locations [29 CFR 1910.307]. Employers should use ground-fault circuit interrupters (GFCIs) on all 120-volt, single-phase, and 15- and 20-ampere receptacles. Wear and tear on electrical equipment or tools can result in insulation breaks, short-circuits and exposed wires. If there is no ground-fault protection, these can cause a ground-fault that sends current through the worker's body, resulting in electrical burns, explosions, fire, or death.The ground-fault circuit interrupter, or GFCI, is a fast-acting circuit breaker designed to shut off electric power in the event of a ground-fault and prevent injury to the worker.
Additional Information:
Electrical. OSHA Safety and Health Topics Page. 1910.305, Wiring methods, components, and equipment for general use. OSHA Standard. 1910.333, Selection and use of work practices. OSHA Standard. 1910.335, Safeguards for personnel protection. OSHA Standard. Preventing Fatalities of Workers Who Contact Electrical Energy. US Department of Health and Human Services (DHHS), National Institute for Occupational Safety and Health (NIOSH) Alert, (1986). Prevention of Electrocutions in Fast Food Restaurants. US Department of Health and Human Services (DHHS), National Institute for Occupational Safety and Health (NIOSH) Alert, (1984). Electrical Safety-Related Work Practices--Inspection Procedures and Interpretation Guidelines. OSHA Directive STD 01-16-007, (1991, July 1). Preventing Electrocutions Due to Damaged Receptacles and Connectors. US Department of Health and Human Services (DHHS), National Institute for Occupational Safety and Health (NIOSH) Alert Publication. No. 87-100, (1986, October).
Protective Equipment:
Power lines should not be repaired or otherwise accessed without adequate Personal safety equipment unless the worker personally verifies that the line is deenergized and properly grounded. Workers must be specifically instructed to wear proper protective equipment, such as gloves and sleeves, required for the task to be performed. Linemen must be instructed to treat all power lines as energized unless they personally deenergize them by establishing a visible open point between the load and supply sides of the line to be repaired, by opening a fused disconnect, by opening a fused switch, or by removing a tap jumper if the load permits. Workers must verify that the power lines have been deenergized. Workers must provide proper grounding for the lines. Unless a power line is effectively grounded on both sides of a work area, it must be considered energized even though the line has been deenergized. Lines must be grounded to the system neutral. Grounds must be attached to the system neutral first and removed from the system neutral last. If work is being performed on a multiphase system, grounds must be placed on all lines. Lines should be grounded in sight of the working area and work should be performed between the grounds whenever possible. If work is to be performed out of sight of the point where the line has been deenergized, an additional ground should be placed on all lines on the source side of the work area.
Detection of Low Voltage:
Persons working on or in the vicinity of power lines should be provided with appropriate safety and protective equipment and trained in procedures that address all magnitudes of voltages to which they may be exposed. Procedures should be established to perform a dual voltage check on the grounded load and supply sides of the open circuit. Once the "fuzzing" method has determined that high voltage is not present, low voltage testing equipment, such as a glowing neon light or a light-emitting diode, should be used to determine if lower voltage is present.
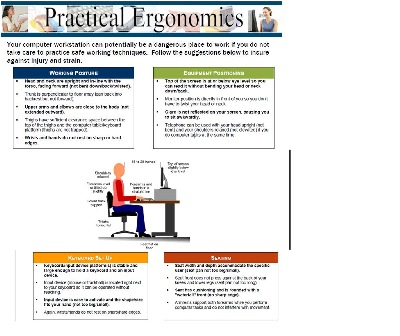
ERGONOMICS, UNIVERSAL PRECAUTIONS:
Health Care-Associated Infections :
ackground
Health care–associated infections (HAIs) are the most common complication of hospital care. According to the Centers for Disease Control and Prevention (CDC), nearly 1.7 million HAIs occur yearly, leading to approximately 99,000 deaths every year. Such infections were long accepted by clinicians as an inevitable hazard of hospitalization. However, recent efforts have demonstrated that relatively simple measures can prevent the majority of common HAIs, and as a result, hospitals and providers are under intense pressure to reduce the burden of these infections.
Four specific infections together account for more than 80% of all HAIs: Surgical site infections (SSI) Catheter-associated urinary tract infections (CAUTI) Central venous catheter–related bloodstream infections (CRBSI) Ventilator-associated pneumonia (VAP)
These infections are especially common in intensive care unit (ICU) patients, and consequently, much recent work has focused on preventing HAIs in the ICU setting. In addition, preventing the transmission of antibiotic-resistant bacteria such as methicillin-resistant (MRSA) has become increasingly important.
Preventive Measures
Effective measures exist to prevent the most common HAIs. The Table shows the strategies currently recommended by the CDC for prevention of SSI, CAUTI, CRBSI, and VAP.
CONTINUED IN: SEE HIPPA COMPLIANCE TOPIC:
